 Helen, Heading Out (1)
Helen, Heading Out (1)
A series of articles about recreating identity after an all-consuming career
By Helen
University Professor of English and Women’s Studies
Retired August 2012 at age 63
Retirement can be an earned and anticipated culmination. Or, as almost happened to me, it can arrive prematurely, as an unwelcome shock.
When I began tenure-track work at the University of Lethbridge in 1980, I was thrilled that someone would pay me to play with literature and vowed fiercely that I would not stop at age 65, despite the mandatory retirement laws of the time. In November of 2002, two universities later, at the age of 53, I took a short-term, and then extended, medical leave. During the almost three years that followed, I could not imagine how I would ever face the classroom or the research again.
Trouble on three fronts
Three circumstances intervened. In March of 2002, my mother died of end-stage liver disease after a two-year illness, involving extreme changes in condition, numerous ambulance trips, and a 24-hour coma one year before she died. My father was her primary caregiver and wore himself out, spending almost 200 days at the hospital. But, although my siblings were many and involved, I lived nearest, twenty minutes away, and served as main support and communications headquarters. And after my mother’s death, my father needed help. Death and I, moreover, have never been on good terms.
Our daughter hit puberty, and the craziness that ensued led, in January of 2002, to our finally getting her a diagnosis of Alcohol-Related Neurodevelopmental Disorder (or Fetal Alcohol Spectrum Disorder). Brain damage from pre-natal alcohol is often marked by low frustration tolerance, impulsivity, difficulty with peers, poor judgement, and emotional dysregulation. When the over-stimulation of unsupervised school-bus trips left our daughter too agitated at the school we’d found for her, my partner and I had to take turns driving the hour and a half round trip twice daily. The search for help before and after diagnosis, from dozens of professionals and social-service agencies often surprisingly ignorant of FASD, was as painful and frustrating as the extreme behaviours that made life at home almost impossible.
My department, which had been uncharacteristically amicable, though a place of self-inflicted overwork, took a turn towards suspicion and hostility, triggered apparently by a committee decision I’d helped to make. Meetings became places of tension, accusation, and obstructionism. I began to feel my own classroom invaded by surveillance and judgement. An earlier dysfunctional department, in Lethbridge, left me more vulnerable to this deterioration in my work environment.
When soldiering on doesn’t work anymore
I would have described my condition as one of stress and exhaustion. Desperation, if you like. A psychiatrist used less welcome language, declaring that the medication I’d been prescribed was inadequate to treat major depression. When competence is the hallmark of one’s identity, mental illness feels stigmatizing. Hell, it feels stigmatizing under any circumstances. But an underlying factor was my predisposition to depression, experienced twice earlier, once as an undiagnosed postpartum episode, and then twelve years prior to my latest crisis, when I had found myself in a new country, in a new job at a vibrant university, with a newly adopted daughter, having left the embattled Lethbridge department I’d been attempting to chair. Back then, with therapy, a brief course of anti-depressants, and a certain amount of teeth-gritting—how could I possibly collapse in a new job?—I’d soldiered on.
I have almost never called in sick at work. I’ve sat down suddenly in class to prevent fainting, while pregnant. I’ve taught after being up most of the night with another gall-bladder attack, cautioning students that I might be a bit woozy from “Demerol and cocaine—I mean codeine.” With mononucleosis as a young academic, I was back at work while still needing to lean up against walls to stand. So why couldn’t I soldier on this time? (The work-warrior behaviour just detailed might itself suggest a clue.)
In a bad place
The University’s biennial Tenure and Promotion Committee had warned the Dean the previous fall that my coordinating Women’s Studies with only one course relief and a quarter-time assistant left me at high risk for burnout. For several preceding years, I’d experienced memory loss and attention problems severe enough to send me to neurologists, endocrinologists, and gerontologists. I’d forget colleagues’ names. I’d have to elicit from students the name of the protagonist in a novel I’d been teaching for thirty years. I’d turn to the blackboard hoping the technical term I wanted would spring to my lips in time.
I couldn’t write a cheque without mismatching the numerical and written amounts or failing to sign it or using my birth year as the date or sending the cheque to the wrong company. I had to make notes of words I’d need, before making a phone call. I went to appointments at the wrong social worker’s, arrived at class with the wrong texts, made bizarre word substitutions in speech and writing. On the road, I was at risk of misreading an advance green, running a stop sign, or overshooting the intersection where I wanted to turn.
Not finding the key as I struggled to get into my office with an armload of books could undo me. I’d even had to cover my face in a departmental meeting when our new Chair made a compassionate remark about our difficulties. Unable to order books, create reading packets, or organize speakers for the next semester, I would obsessively clean my desk or cull my files. When a close colleague at a Quebec City conference mentioned her fear that her plane might go down, I told her that I’d rather hoped mine would and that I’d already wept three times that day in various washrooms. Her refusal to take my state lightly was a catalyst forcing me to make a sober assessment.
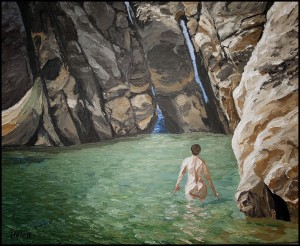
Taking Flight
My doctor asked me if I would be better keeping my hand in with only a part-time leave, but I’d let things go too far for anything but flight. Her insistence then was that I go on leave immediately. Before I could do that though, because I was coordinator, I had to interview, hire, and orient my own teaching replacement for a forthcoming senior course in Women’s Studies.
For most of the next three years, I was in a bad way. I couldn’t read a light, popular novel. The prospect of having, in time, to keep up with the new research even on my favourite authors appalled me. I felt revulsion at the complex literary theory central to my discipline. I’d moved far beyond the “games” of my early career, of finding recurring images or textual patterns. Although my field had become socially and politically engaged with issues of colonization, gender, race, poverty, and sexuality, however, I was sickened by the pointlessness of my work.
While I was never actively suicidal, my brain worked independently at elaborating possible ways of ending the pain (high balconies, roadside cliffs, pharmaceuticals, razor blades). Because I was able to get out of bed and didn’t feel the absolute evacuation of life’s colour described by some depressives, I felt fraudulent about my diagnosis. But I was seriously incapacitated. I had a therapist who refused to allow me to see myself as permanently disabled. But just months before I resumed work, I experienced chest-crushing anxiety at the prospect of a return.
We faced new expenses. So the reduced income of disability leave, let alone the prospect of a forced early retirement, was alarming. Besides, my skills as a teacher, a researcher and writer, even an administrator had been central to my identity since adulthood. My work, in many ways, was who I was. And now I couldn’t get far enough away from it.
Clearly I needed to have found better strategies for absorbing the personal and workplace pressures that had cracked me. Or I would need to discover them now if I hoped to re-emerge. And perhaps for some of you who may recognize familiar moments in my saga thus far, the account of my emergence, in my next installments, will help avert a similar crisis.
Retirement, I’d argue, feels better when it is chosen.
Helen, this is brilliant! Beautiful in its honesty. Your description makes me feel your pain. Thank you.
Thanks, Amy. I figure we should share such things, so people feel less alone.
Helen, this is vivid and searing, both rich and concise — and what an image of the “cognitive” effects of “emotional” issues! Superb, eloquent and touching. You’ve also helped me to understand and put names of some periods of my life. I do feel less alone, even though I’m not in that space right now, I know it’s in me because I’ve been there and could go back again some day.
Thanks, Ann. Yes, the cognitive effects were puzzling for years for me and my doctor, who actually consulted with a doctors’ group about my problem. It is a hard place to be, as you know.